colonoscopy
Colonoscopy
What is a colonoscopy?
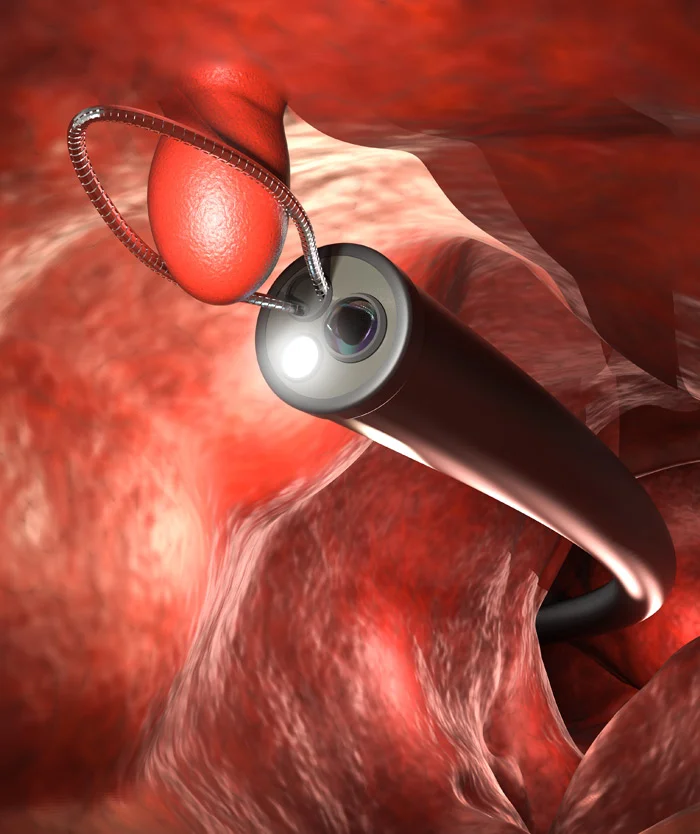
A colonoscopy is a procedure your GI doctor performs to examine the lining of your colon (large intestine). The doctor will insert a flexible tube into the rectum and through the colon, to look for abnormalities such as colon polyps.
To prepare for a colonoscopy, your doctor will give you a specific set of bowel prep instructions. It’s important to follow all of the instructions very carefully.
Prior to the procedure, you will be given a sedative and pain medication through an IV. Following the procedure, you will be groggy for a few hours and therefore, should not schedule anything else for the remainder of the day.
You are NOT allowed to drive for the remainder of the day. It is recommended to have a person over the age of 18 stay with you for 6-8 hours after the procedure.
Please note, it is your responsibility to contact your insurance company about coverage and cost for your upcoming colonoscopy procedure. Sometimes colonoscopies result in a cost to the patient. Be sure to state to the insurance company when your last colonoscopy was and if you have a personal history or family history of colon cancer or polyps.
Explore our colonoscopy billing page to learn more about the billing process.
Why is Colonoscopy Considered The Gold Standard?
A colonoscopy is the only test that can detect and prevent colorectal cancer by finding and removing polyps immediately during the procedure.
Because of this kind of capability that can both detect and treat colon cancer with a high degree of accuracy, it has earned the gold standard reputation.
Another key factor that differentiates colonoscopy from other tests lies in its early detection abilities.
What is the difference between a screening test and diagnostic colonoscopy?
A single colonoscopy can therefore be both a screening test – that finds undiagnosed symptoms, as well as a diagnostic procedure – that finds the cause of symptoms.
If you choose a screening test – not a colonoscopy, and the result is positive (abnormal), you will then need an additional follow up colonoscopy to remove the polyps. You may then be charged for this additional procedure as it is now identified as a diagnostic colonoscopy.
Colonoscopies also have an extremely high detection rate of colon polyps which contributes to a higher survival rate among early colorectal cancer diagnosis. This is because we use state-of-the-art medical devices like GI Genius, which uses AI to detect colon polyps hidden to the human eye. These are some reasons why a colonoscopy is still considered the gold standard for detecting and preventing colorectal cancer.
Learn more about why colonoscopies are the gold standard.
Our highly trained gastroenterologists provide colonoscopies in Denver and surrounding cities. We operate seven GI clinics in the Denver and Boulder area. Find a convenient location near you by visiting our locations page.
Check this blog post – 8 Myths About Colorectal Cancer and Colonoscopy Screening
Colonoscopy FAQs – Questions & Answers
Will I be charged for my colonoscopy?
To answer this question, we need to address the difference between a preventive, or screening colonoscopy, and a diagnostic colonoscopy:
- The cost of a preventive, or screening colonoscopy, is generally covered by your insurance under the Affordable Care Act.
- The cost of a diagnostic colonoscopy is generally NOT fully covered by your insurance, you may have to pay the deductible and copay.
What is a preventive, or screening colonoscopy?
A preventive or screening colonoscopy is performed on an asymptomatic patient to test for the presence of colorectal polyps or cancer.
Preventive or screening colonoscopies are performed on patients who:
- Are 45 years of age or older (50 years of age for some insurances)
- Do not have any gastrointestinal symptoms (i.e., abdominal pain, diarrhea, rectal bleeding)
- Have not had a colonoscopy within 10 years
- Do not have a personal or family history of colon polyps or colon cancer (coverage is plan-specific, some screenings may include family history)
*You may also be charged for some additional colonoscopy services according to the cost sharing provisions in your individual health plan. Contact your insurance company to determine your individual benefits and possible out-of-pocket costs for your colonoscopy.
What is a diagnostic colonoscopy?
A diagnostic colonoscopy is performed on a patient to evaluate abnormal findings or symptoms.
Diagnostic colonoscopies are performed on patients who:
- Have gastrointestinal symptoms (i.e., abdominal pain, diarrhea, rectal bleeding) or abnormal imaging of colon (i.e., CT scan, MRI).
- Have a personal history of polyps or have a gastrointestinal disease
- Have a positive Cologuard or FIT test – you must then get a follow-up diagnostic colonoscopy!
*Please contact your insurance company to determine your individual benefits and possible out-of-pocket costs for your colonoscopy.
Do I really need to have a colonoscopy?
The need for a colonoscopy is real. In the United States, colorectal cancer (CRC) is the third most common cancer diagnosed among men and women. CRC largely can be prevented by the detection and removal of adenomatous polyps, and survival is significantly better when CRC is diagnosed while still localized. (Medical Position Statement of American Gastrological Association Institute).
What if a polyp is discovered during a preventive screening colonoscopy?
If a polyp is removed during a preventive screening colonoscopy, future colonoscopies would normally be considered diagnostic because the time intervals between future colonoscopies would be shortened.
Does a colonoscopy hurt?
The doctor gives you pain relievers and a sedative to bring you into a state called “conscious sedation.” This is not like general anesthesia, where you’re unconscious, but a pleasant, sleepy, relaxed dreamlike state.
How will I feel afterward?
After the procedure, you’ll be taken to one of our state-of-the-art recovery rooms where you’ll wake up. Most people feel OK after waking up. Some feel a bit woozy. You’ll be watched closely by one of our nurses. You may have some gas, which could cause mild discomfort and will be asked to pass gas. You will need someone to drive you home after receiving sedation.
I have heard of a virtual colonoscopy, how does it compare to a conventional colonoscopy?
Body imaging of all types has revolutionized the practice of medicine and saves countless lives every day. From the early use of x-rays for visualizing bones to the soft tissue CT and MRI scans that are common today, doctors are able to see and understand more so that they can do more.
Virtual colonoscopy (also known as CT colonography), a relatively newer use of CT scanning, is one such technique. It enables a radiologist to examine the colon for polyps that could become cancerous, thus potentially averting colon cancer.
In essence, it is a colon cancer screening technique that can be used as an alternative to traditional, optical colonoscopy, a technique that was first employed in 1969. This traditional technique has been perfected continually over those 40 years and remains the “gold standard” for colonoscopy. Optical colonoscopy (i.e. standard colonoscopy) is typically performed by a gastroenterologist who specializes in the digestive tract.
There are other tests that can determine the presence of colon cancer, but only a colonoscopy – virtual or standard – can spot polyps throughout the length of the colon before they become cancer.
If you are a candidate for a screening colonoscopy (the American College of Gastroenterology recommends screening for everyone at age 50; younger if a first degree relative has had colon cancer), should you have a standard colonoscopy or consider a virtual colonoscopy (also known as a CT colonography)?
Consider the following:
- All colon cancers start out as polyps
- Polyps can be removed during a standard colonoscopy but they cannot be removed during a virtual colonoscopy
- Removal of polyps is the only way to prevent colon cancer
- The National Cancer Society says it is not possible to identify which particular polyps will turn into cancers
If you are over 50 you have a 40 percent chance of having polyps. In other words, should you choose a virtual colonoscopy and you are in the 40 percent group, you will have to schedule a standard colonoscopy to have those polyps removed. This means scheduling an appointment with a gastroenterologist and repeating the colon cleansing process that is required with both procedures. Why go through the process twice? And why delay the removal of potentially cancerous polyps?
Virtual colonoscopy (CT colonography) uses radiation. This radiation exposure may increase your long term risk of developing cancer. Moreover, because of the uncertainty associated with virtual colonoscopy’s ability to detect smaller polyps, more frequent follow up exams are recommended, compounding radiation risk. Standard colonoscopy involves no radiation.
After a thorough review of data, Medicare concluded that there was inadequate evidence to show that virtual colonoscopy is appropriate for colorectal screening. Likewise, the Colorado Clinical Guidelines Collaborative and the U.S. Preventive Services Task Force identify standard colonoscopy as the preferred colorectal screening method except in those limited circumstances where standard colonoscopy is not feasible.
Virtual colonoscopy is not covered by Medicare or most private insurance except in limited cases where optical colonoscopy is not feasible. Most insurance plans cover a straightforward screening standard colonoscopy if you meet the age and/or family history criteria outlined above. And, it will cover any follow-up colonoscopies based on your gastroenterologist’s recommendation.
All of the Gastroenterology of the Rockies physicians are board certified gastroenterologists who received advanced training in performing standard colonoscopies and removing polyps. They perform hundreds of colonoscopies each year.
What if the doctor finds something?
The doctor will remove polyps because they could eventually become cancerous. If your doctor sees a large polyp or tumor or anything else abnormal, a biopsy will be done. For the biopsy, a small piece of tissue is removed. Having a biopsy is painless, because the inner lining of the colon has no pain receptor nerves.
Will I be in a private room?
A colonoscopy is always done behind closed doors, in a private room, with no other patients around. Your privacy is a top concern.
Will I be unconscious during the procedure?
Before the exam, your doctor administers pain relievers and a sedative through an intravenous (IV) line. The sedative brings you into a state called “conscious sedation.” This is not like general anesthesia, where you’re unconscious, but a sleepy, relaxed dreamlike state.
How often do I need a colonoscopy?
Your doctor will suggest how often you need this exam, depending on your personal risk for colon cancer. Doctors usually recommended starting at age 50 and repeating it every 10 years. If you have an increased risk for colon cancer, or have had previous treatment for colon polyps or colorectal cancer, the test may be done at a younger age and more often. Find out from your doctor whether you should start before age 50.




