
Gut Health Feeds Mental Health
Gut Health Feeds Mental Health – What Women Need to Know
Have you ever wondered why gut health feeds mental health? Now that more people talk about mental health, stress and work life balance, we finally get to have more open discussions about these important topics. And that means we will find better solutions that work for us–while keeping our well-being and quality of life in mind.
As we celebrate Women’s Health Month and Mental Health Awareness, let’s dive right into these topics.
As you’re well aware, there’s a strong connection between our brain and stomach—commonly referred to as the gut-brain connection or gut-brain axis. So it’s not that unusual to think about how our mental wellness can affect digestive symptoms like Irritable Bowel Syndrome (IBS) and digestive disease like Inflammatory Bowel Disease (IBD).
Teaming up female healthcare professionals

Considering how a woman’s hormones fluctuate throughout the month, not to mention stress hormones and life’s unpredictable moments, these factors can take a toll on both a woman’s emotional health and physical health. So we wanted to explore these topics in greater depth and find answers for our female readers. We turned to the medical providers on our female gastro services team to dive into this fascinating connection where gut health feeds mental health—from a woman’s point of view.
First up, Dr. Kelly Zucker, board certified gastroenterologist with Gastroenterology of the Rockies. Here are some questions we asked Dr. Zucker.
Question: Why do some female patients prefer working with female providers?

Answer: “I believe patients are more at ease with a female provider because the gastrointestinal system is a sensitive system- often problems with our GI tract manifest as symptoms that aren’t traditionally discussed (flatulence, stooling, bleeding). Having a woman listen, and perform procedures, can provide a level of comfort. Women’s bodies are different–and having someone who can relate to you makes an impact.”
Question: What’s the interconnection between gut health and mental health?
And how might this translate into better self-care at home?
Here’s Dr. Zucker’s response.
Answer: “Our GI system is directly connected to how we are feeling and stressors in our lives. The gut-brain axis is a complex network involving the central nervous system and the GI system. While all mechanisms are not yet understood, we know serotonin receptors in the

gut are partially mediated by the central nervous system- i.e., more stress, more GI symptoms. I believe self-care at home, mainly minimizing stressors, or talking with a therapist helps greatly with GI symptoms. Getting enough sleep and eating whole foods is always, always a plus!
Myth or Fact? Are women more prone to constipation and bloating than men?
And, is it true that anatomy, motility and hormone levels play a role in constipation? Or are there other contributing factors?
Here’s what Dr. Zucker had to say about women who experience constipation.
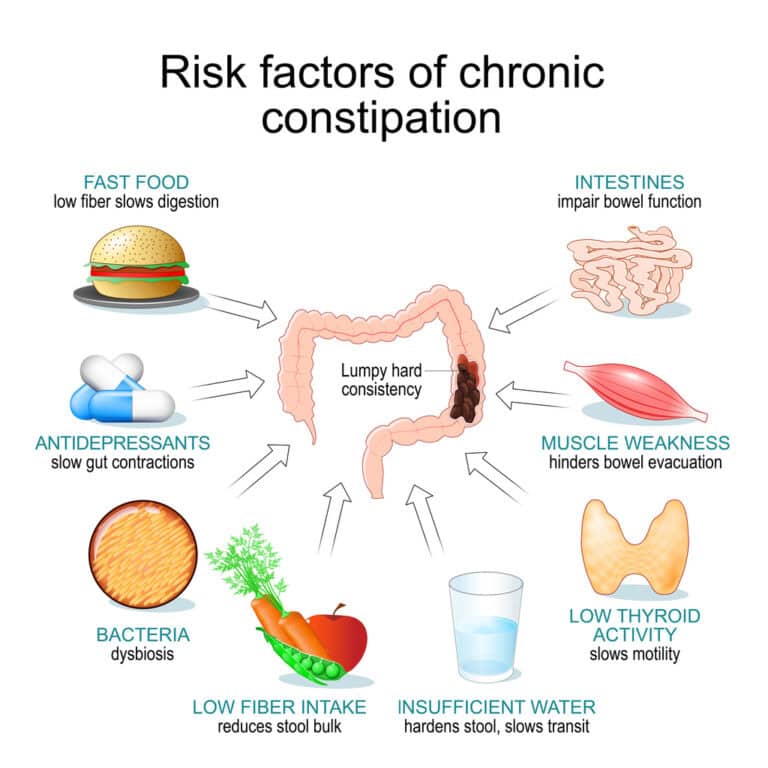
Answer: “Yes, it is true women are more prone to constipation and bloating! Several factors associated with this increase are noted, mainly serotonin (dysregulation implicated in IBS), sex hormones (estrogen and progesterone influence GI motility and visceral sensitivity), and the differences in male and female microbiota can influence dysbiosis, meaning an imbalance in the microbiota

Understanding Female Patient Needs – Key for Gut Health & Mental Health
Let’s hear from another GI specialist on our female gastro services team–meet Susan Gieske, PA-C. We asked Susan a few questions about how women may respond to care from our female providers. Here Susan shares her approach to working with female patients in ways that help build rapport and trust.
Question: What do female patients appreciate most in terms of the kind of care they receive?
Answer: “Generally, I find that my female patients appreciate feeling heard and validated, and this is the case from mild GI conditions like mild GERD or IBS, to serious GI diseases like severe Crohn’s and decompensated cirrhosis. Even if it’s “just IBS,” these symptoms can be incredibly impactful to their day-to-day lives. Because functional symptoms are not necessarily dangerous, some patients do not feel heard when discussing symptoms. For many of my IBS patients, they have lived with the stigma of it being “all in their head” – and I try to emphasize that symptoms are symptoms regardless of where they come from. I think it’s important to ensure every patient understands that I hear their symptoms and care about treating them.”
Question: Why might female patients feel more at ease or trust a female provider?
Here’s a response from Susan Gieske, PA-C.
Answer: “For many women, having a female provider can feel more comfortable, especially during sensative procedures like exams or scopes. A woman’s past experiences, personal boundaries, or trauma histories can all play a role. It’s completely understandable some women may feel more at ease or safer with a female provider, and we fully support each patient’s preference.”
Question: What health tip would you give women who want to take care of gut health and mental health?

Here’s what Susan Gieske, PA-C shared.
Answer: “Brain and gut are very connected. For this reason, mental health can worsen GI symptoms, and GI symptoms can worsen mental health. I find that treating both is important. Eating a healthy diet with lots of fiber can help both the gut as well as mental health. Similarly, treating your mental health (i.e. therapy, medications, meditation) can help GI symptoms. For my patients, I try to make sure we are addressing both GI symptoms as well as their mental health. This is incredibly important for conditions like IBS, but can help with any GI condition.”
Wanting more information about services from our female gastro team? Please reach out to us. Our providers can help you come up with a treatment plan that fits your lifestyle needs. Ask us about ways we can help you improve gut health, nutrition and overall well-being.
Call 303-604-5000 to schedule your consult with one of our GI specialists. We see patients at seven locations from Denver to Longmont.
Produced by Elise Oberliesen, digital marketing specialist; medical review provided by Kelly Zucker, DO, gastroenterologist.




