Varices
 What are Varices?
What are Varices?
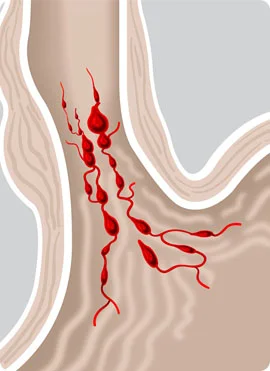
Varices are dilated veins in the esophagus or stomach caused by elevated pressure in the portal venous system, typically from cirrhosis. They may bleed massively but cause no other symptoms.
An upper endoscopy can help diagnose varices and treatment is primarily with endoscopic banding and IV octreotide. Sometimes a transjugular intrahepatic portosystemic shunting procedure is needed.
Symptoms and Signs of Varices
Patients typically present with sudden, painless, upper GI bleeding, often massive. Signs of shock may be present. Bleeding is usually from the distal esophagus, less often from the gastric fundus. Bleeding from gastric varices also may be acute but is more often subacute or chronic. Bleeding into the GI tract may precipitate portal-systemic encephalopathy in patients with impaired hepatic function.
Diagnosis of Varices
Both esophageal and gastric varices are best diagnosed by endoscopy, which may also identify varices at high risk of bleeding (eg, those with red markings). Endoscopy is also critical to exclude other causes of acute bleeding (eg, peptic ulcer), even in patients known to have varices; perhaps as many as one third of patients with known varices who have upper GI bleeding have a nonvariceal source.
Because varices are typically associated with significant hepatic disease, evaluation for possible coagulopathy is important. Laboratory tests include complete blood count (CBC) with platelets, prothrombin time (PT), partial thromboplastin time (PTT), and liver tests. Bleeding patients should have type and cross-match for 6 units of packed red blood cells.
Prognosis for Varices
In about 40% of patients, variceal bleeding stops spontaneously. Previously, mortality was > 50%, but even with current management, mortality is at least 20% at 6 weeks. Mortality depends primarily on severity of the associated liver disease rather than on the bleeding itself. Bleeding is often fatal in patients with severe hepatocellular impairment (eg, advanced cirrhosis), whereas patients with good hepatic reserve usually recover.
Surviving patients are at high risk of further variceal bleeding; typically, 50 to 75% have recurrence within 1 to 2 years. Ongoing endoscopic or drug therapy significantly lowers this risk, but the overall effect on long-term mortality seems to be marginal, probably because of the underlying hepatic disease.
Treatment of Varices
Airway management and fluid resuscitation, including transfusion if needed, is done to manage hypovolemia and hemorrhagic shock. Patients with coagulation abnormalities (eg, significantly elevated international normalized ratio [INR]) can be treated with 1 to 2 units of fresh frozen plasma, but this should be given cautiously because giving large volumes of fluid to patients who are not hypovolemic may actually promote bleeding from varices. Patients with known cirrhosis with GI bleeding are at risk of bacterial infection and should receive antibiotic prophylaxis with norfloxacin or ceftriaxone.
Because varices are invariably diagnosed during endoscopy, primary treatment is endoscopic. Endoscopic banding of varices is preferred over injection sclerotherapy. At the same time, IV octreotide (a synthetic analog of somatostatin, which may also be used) should be given. Octreotide increases splanchnic vascular resistance by inhibiting the release of splanchnic vasodilator hormones (eg, glucagon, vasoactive intestinal peptide). The usual dose is a 50-mcg IV bolus, followed by infusion of 50 mcg/hour. Octreotide is preferred over previously used agents such as vasopressin and terlipressin, because it has fewer adverse effects.
